Coronary Artery Disease: Options in Surgical Procedure
Current surgical procedures for Coronary Artery Disease include Coronary Angioplasty Stent Placement, Coronary Artery Bypass Graft (CABG), and a heart transplant procedure. According to NHS article Treatments: Coronary Artery Disease, Coronary Angioplasty is a procedure where a small balloon is placed within the clogged artery and blown up until the fatty tissue is pushed. Then, a metal stent is put in its place to hold it open. Coronary artery bypass grafting, or CABG, is when a new blood vessel, either from another part of the patient’s body or a lab-grown one, replaces the clogged vessel. Lastly, if cases get too severe and the heart is no longer able to function alone, patients would enter a heart-transplant procedure, where surgeons would replace the faulty heart with a healthy one from a donor. (NHS, Treatments: Coronary Heart Disease). Traditionally, in a CABG procedure, a large incision in the chest is made that briefly stops the heart, while using a Heart-Lung bypass machine is used to pump blood throughout the body while the heart is stopped. Developed during the 1990’s, off pump procedures were developed for this procedure. Furthermore, other minimally invasive procedures exist today such as keyhole surgery and robotic procedures are available today. (John Hopkins University, Coronary Artery Bypass Graft Surgery)
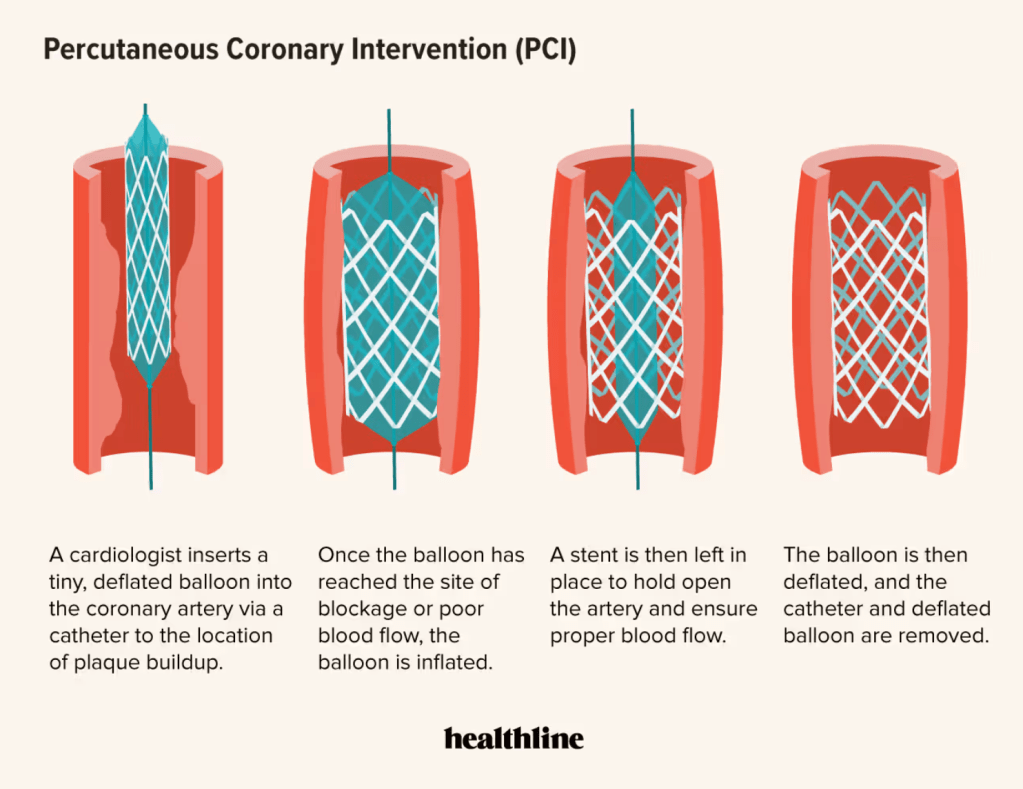
Figure 1: Vessel before and after having a PCL
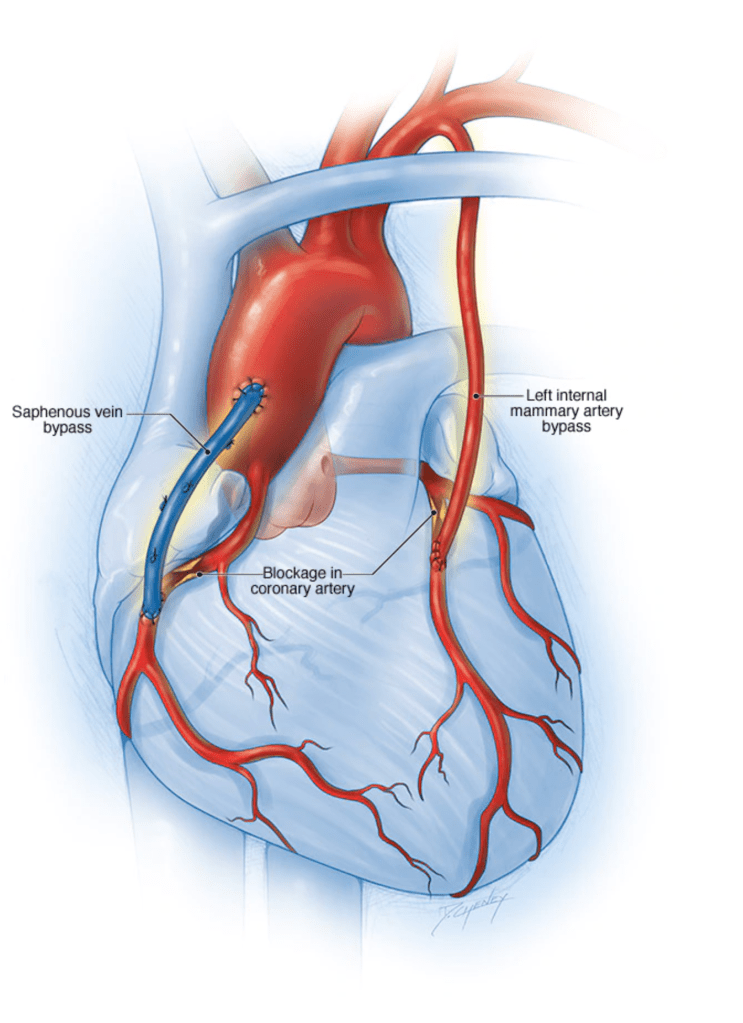
Figure 2: CABG using a saphenous vein in the leg and left internal mammary artery in the chest
Bypass Procedure Summary and the Case of Sally Smith
According to Dr. Bhavik Patel, a cardiothoracic surgeon at UnityPoint Health, stenting and CABG are both procedures to increase the blood flow to someone’s heart. Stenting is done through the blood vessel, where they open up a blockage using a metal cage while bypass surgery is done from the outside of the heart using a replacement vessel. Stenting is generally less invasive and is a shorter procedure with less risk while CABG is an open heart surgery where they are able to address more complicated blockages and has a better long-term outcome, however it is tougher to recover. Usually, while younger and healthier patients tend to lean toward open heart surgery due to its long-term benefits, older patients who are more frail tend to choose stenting.
However, for Sally Smith, an example patient of age 60 and over, there are particular factors to be considered in choosing the CABG procedure over PCI. One of these factors lies in the physiology change in the small and large vessels in the heart, reducing physiological reserve according to Arun Natarajan’s article Coronary Artery Bypass Surgery in Elderly People. There are two main areas in which these changes occur: the intimal layer of vessel wall where they become less smooth over time, and in the myocardium where deposition of connective tissue, calcium, and lipids cause the ventricle to remain stiff, reducing diastolic volume by one third to one half compared to a 20 year old. Therefore suggesting patients can benefit from CABG with long-term survival and a good quality of life after the procedure by providing a replacement blood vessel instead of treating the old one. (Natarajan, PMC)
According to Nature’s scientific report on comparing outcomes between CABG and PCI, there was a lower late mortality rate in CABG procedures and there is significantly lower risk of deaths in the follow-up compared to PCI. PCI focuses more on treating flow-limiting lesions, as it cannot be expected to significantly limit new myocardial infarctions (MI). On the other hand, CABG is able to do this by bypassing many coronary lesions, causing “collateralization,” to the grafted vessel and other coronary arteries that may prevent myocardial infarctions from rupture. (Nature, Comparing Outcomes Between Coronary Artery Bypass Grafting ) Due to this benefit of lessening the infection risk, and risk consideration in treating the original compromised artery, CABG may be considered a better option for Sally’s case.
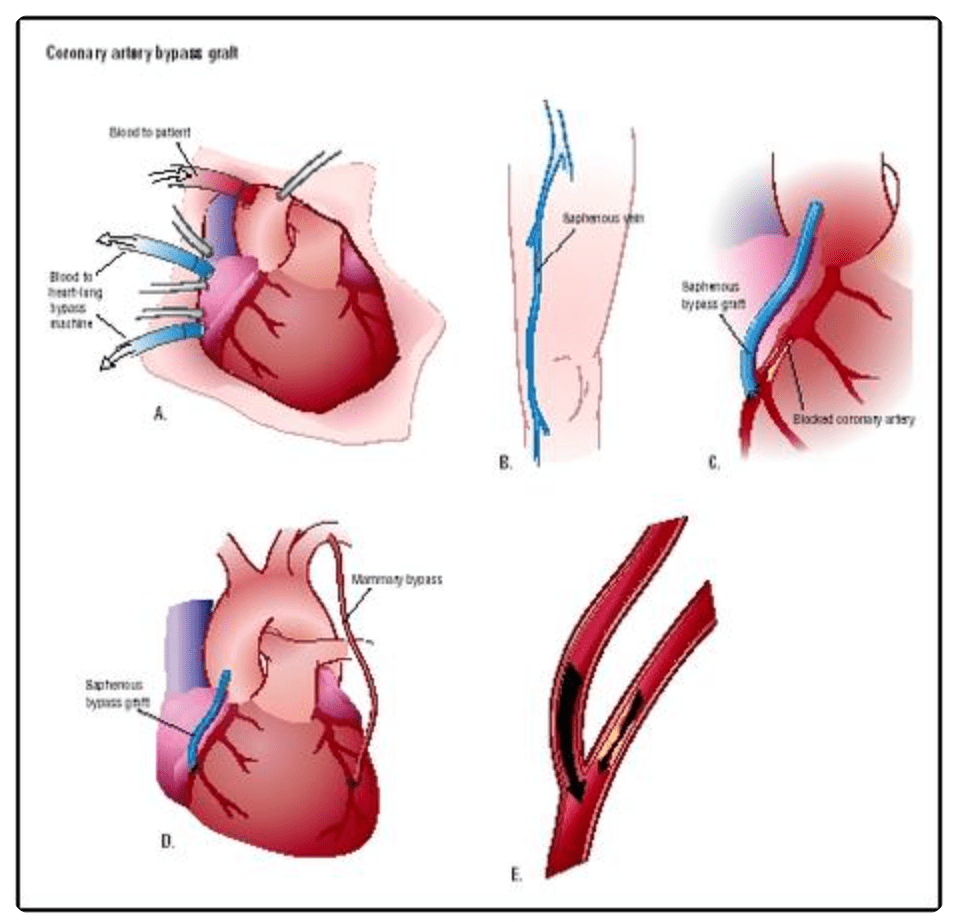
Figure 3: llustration of the CABG procedure. A.) Chest is opened to visualize the heart, and a heart-lung machine is used in place to the function of the heart. B.) A segment of the Saphenous Vein is removed. C.) The vessel is used to bypass a blockage of the coronary artery, attaching to the aorta past the point of blockage. D.) Both Saphenous Vein or Internal Mammary Arteries provide options for the material. E.) Bypass vessels provide an increase of blood flow to the area affected by the original coronary artery.
Overview of Current Technology and Material
According to AHA/ASA Journal’s article Bioengineering Human Tissues and the Future of Vascular Replacement, traditional vascular grafts are made of synthetic polymers, animal and cadaveric tissues, or autologous vasculature. These technologies have been around for some time with many benefits, and observations have been made addressing their limitations such as durability and long-term patency, susceptibility to infection, risk of rejection, and inflammatory and mechanical failure. Constructing vascular conduits such as blood vessels, viable autologous cells as well as decellularization, provide the future for developing materials that are safer and have better durable performances. Some of the current replacement materials include the following: (Naegeli et. al. AHA/ASA Journals)
- Synthetic Conduits
- Autologous Blood Vessels
- Xenografts (Bovine or Porcine)
- Cadaveric Allografts
- Tissue-Engineered Vascular Grafts
Synthetic Conduits
Synthetic Conduits are non degradable polymer vascular grafts that can be made of PTFE (gore-tex), PET (polyethylene terephthalate). Benefits of these synthetic grafts include relatively inexpensive cost and production, readily available, and long shelf life. PTFE is defined with its characteristic of its porosity, where higher porosity yields a greater potential for tissue ingrowth endothelialization (the lining of the cell). Disadvantages of PTFE is the problematic long-term patency relating to susceptibility to infections such as thrombosis, information and risk of rejection. Another example is Dacron, a textile vascular graft made of polyethylene terephthalate fiber, providing lower permeability, less bleeding, promotes greater tissue ingrowth and is more compliant to its host. However, long term patency remains a limitation. The third kind of synthetic tissues is PU, consisting of copolymers of 3 different monomers: a hard crystalline segment that provides rigidity, a polymer chain extender, and a soft, flexible segment of polyester, polyether, or polycarbonate for flexibility. The issue with this material is its structural failure linked to enzymatic attacks, oxidative stress, and stress cracking, leading to the risk of thrombosis infection. (Naegeli et. al. AHA/ASA Journals)
Figure 4: Image of a synthetic Conduit after implantation.
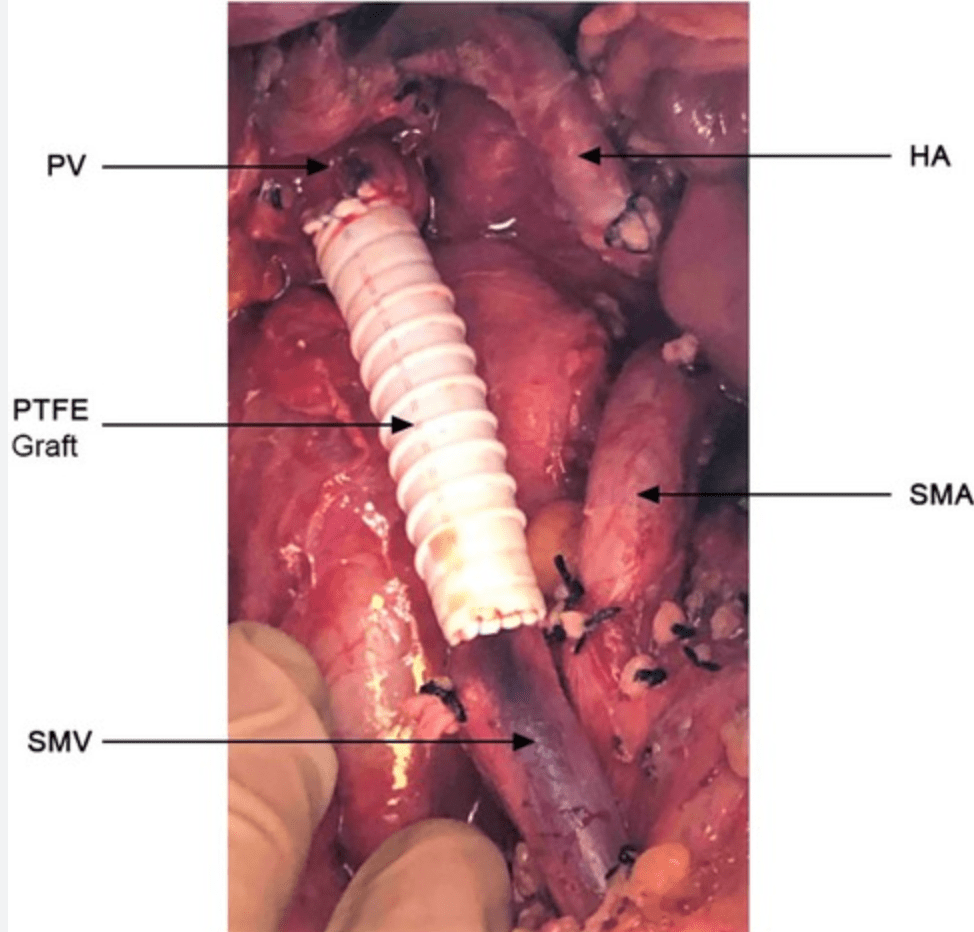
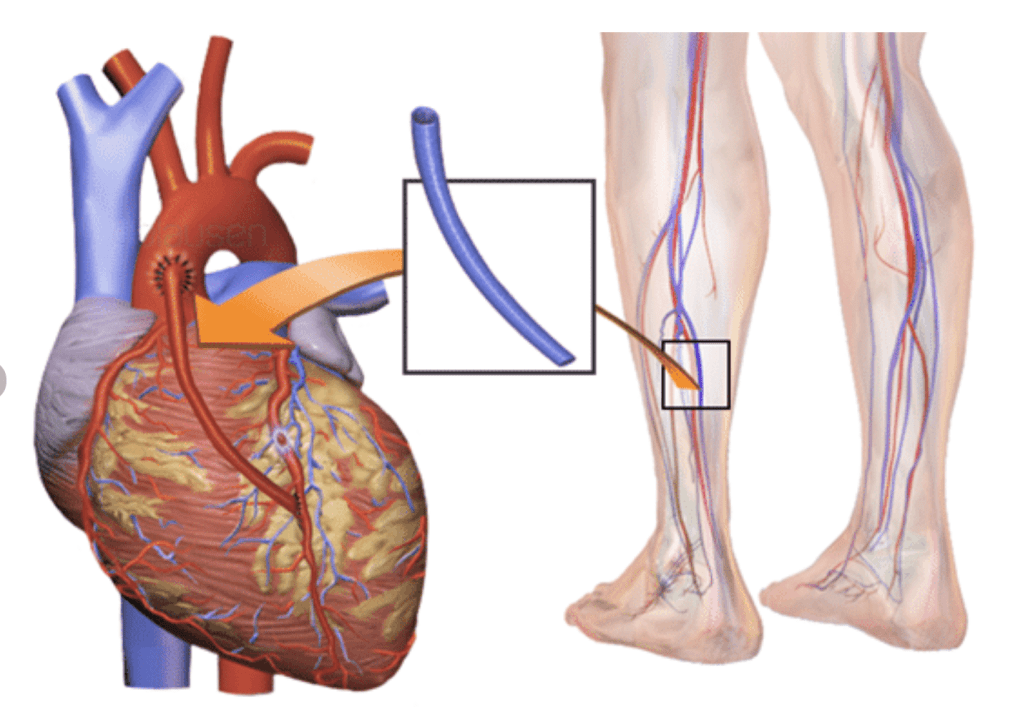
Figure 5: Image of a Saphenous Vein used as a replacement vessel for the heart.
Autologous Blood Vessels
Autologlous Blood Vessels are vessels taken from the patient’s own body, with the most common candidate being the Internal Mammary Artery (IMA) or Saphenous Vein (SV). Autologous Blood Vessels are preferred due to their excellent long-term patency rates and the elimination of risk of rejection. They have physiological properties that are closest to the original compromised vasculature. According to the American College of Cardiology guidelines, IMA has a superior performance in CABGs over SV due to its anatomic structure, which provides an elastic artery with elastin unevenly distributed in its structure.The IMA’s endothelium has fewer fenestrations and lower permeability when compared to SV, preventing lipoproteins from entering the sub-endothelial space which can cost inflammation and intimal hyperplasia. Furthermore, IMA can be accustomed to the high-pressure arterial flow of the aorta-coronary circulation with its size similar to the original vasculature, contributing to its long-term patency. However, in other cases such as PAD revascularization, the use of autologous SV is recommended over synthetic materials such as PTFE of Dacron for it provides better patency
rate and reduced risk of reintervention. The Structure of SV has the intima lined by an endothelium on a fenestrated basement membrane that is more susceptible than IMA to injury during harvesting, storage and implantation. Efforts has been made to limit the damage inflicted to endothelium of harvested veins, with development such as DuraGraft, a PH-Balanced physiological salt solution containing elements that minimize the risk of neointimal hyperplasia stemming, providing a flushing and storage solution that protects the structural and functional integrity of the vascular endothelium. (Naegeli et. al. AHA/ASA Journals)
Cyropreserved Cadaveric Allogenic Veins (CVG)
CVGs serve as an alternative when synthetic grafts are not practical and when autologous veins are unavailable. CVGs are cryopreserved in specialized storage where practical limitations exist in the planning and preparation, where the performance of endothelium is decreased during the harvesting and storage procedure. The presence of viable allogeneic cells triggers an immune response from the host that can jeopardize patency and affects the chance of success of future organ transplant. With primary limitation in poor patency rate and high risk of thrombotic infection, CBF serves only as an alternative in CABGs. (Naegeli et. al. AHA/ASA Journals)
Xenogenic Cardiovascular Grafts (Xenograft)
Xenografts are vessels sourced from animals, typically Bovine or Porcine (pigs or cows), and processed to make them suitable for human use. Xenografts are used primarily when autografts or allografts are not available. The main benefits of the use of Xenografts is the abundant supply of this biological tissue that is “strong, pliable and durable.” All vascular xenografts are decellularized to lower the risk of immunogenic potential of the graft, however, its efficacy and durability varies tremendously depending on its application. For example, the use of Cormatrix (porcine small intestinal submucosa) or Artegraft (bovine carotid artery) have proven adequate performance compared with autologous and synthetic types. However, the use of Xenografts in cardiac application has a high rate of reintervention and failure relating to mechanical failures of the materials, which is mainly due to the high-pressure requirement in arterial grafts that limits use of the lower pressure nature of arteriovenous grafts. Furthermore, inflammation and fibrosis infection have been observed frequently in high-pressure environments with high mechanical stress such as in cardiac related application. (Naegeli et. al. AHA/ASA Journals)
Tissue-Engineered Vascular Grafts (TEVG)
TEVGs are designed to address the growth time, wound care, and operating time of harvesting autologous cells, veins or arteries. The mechanical and structural properties of replacement vessels can be designed to handle the arterial system’s high-pressure environment with low-permeability, and can perform similar to autologous vasculature in terms of risk of infection and mechanical failure. The first TEVG was produced in vitro with vascular cells in 1986 with a structure made of collagen gel tube supported by a Dacron sleeve jacket. With years in development, TEVG can be produced today in the method of harvesting peripheral veins from a patient for vessel wall cells expansion that forms the TEVG, seeding scaffolds using autologous cells such as bone marrow cells. This procedure is deemed very versatile to produce many types of tissues. The future of tissue engineering vascular grafts can include multiple paths of development including in vivo generation, cell reprogramming, lumen coatings, and gene therapy. (Naegeli et. al. AHA/ASA Journals)
Figure 6: Diagram of the approach in which TEVG is produced.
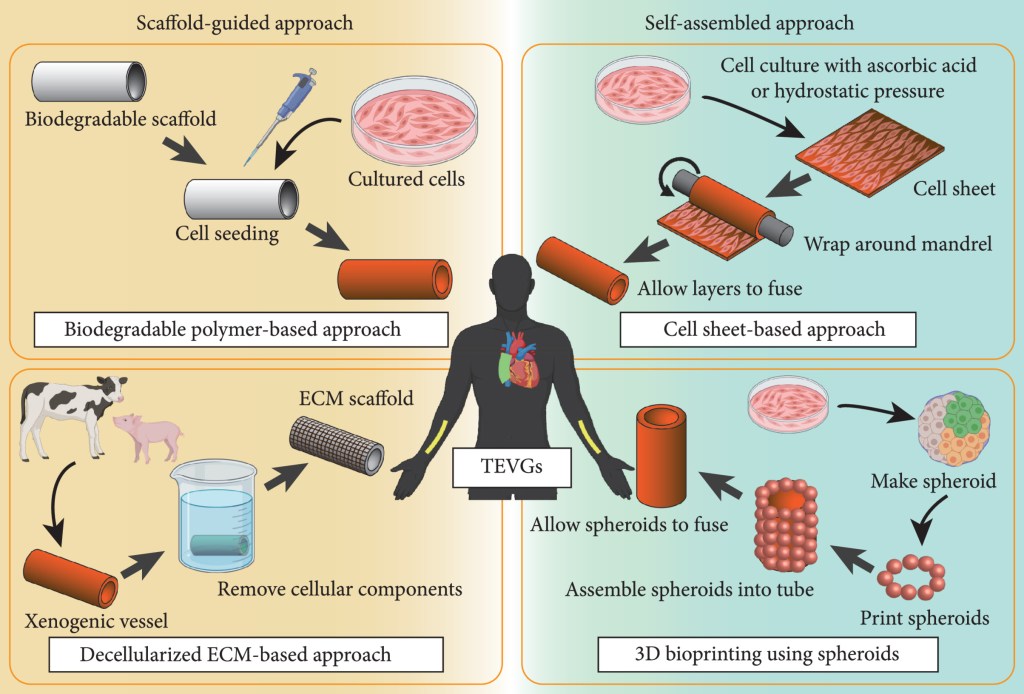
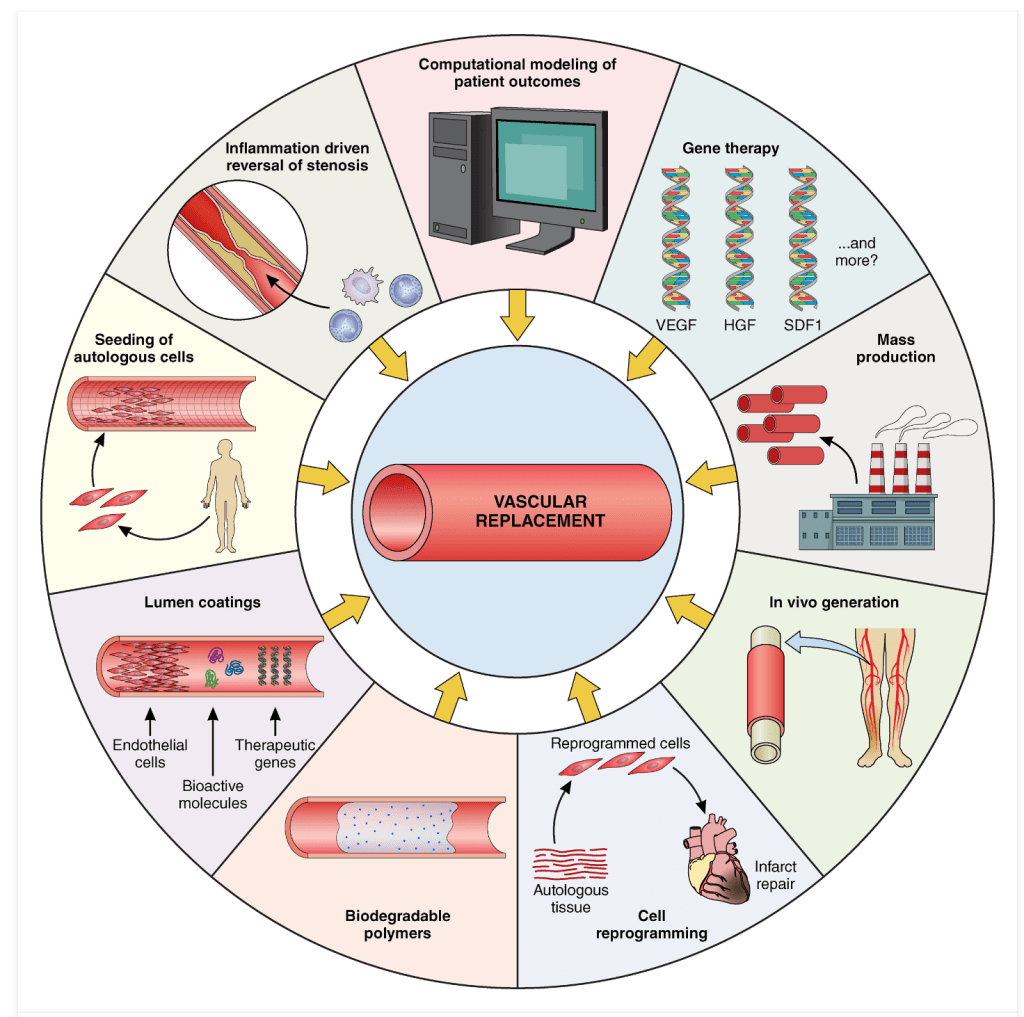
Figure 7: Illustration showing multiple avenues of research continued to advance the field in engineering or vascular grafts.
Criteria for Design Success
Seven criteria are identified to evaluate the success for each product design, including the product’s Longevity/Durability, Mechanical/Structural Integrity, Risk of Infection, Risk of Host Rejection, Growth/Recovery, Availability, and Cost to Harvesting/Production.
| Factor/Types | Weight (1-10) | Synthetic Polymer | Autologous Vessels | Xenografts | TEVG | |
| Longevity | 10 | 10 | 7 | 3 | 9 | |
| Mechanical/Structural Integrity | 10 | 8 | 9 | 5 | 6 | |
| Resistance to Infection | 10 | 4 | 9 | 6 | 9 | |
| Compliacne/Low Rejection | 10 | 4 | 10 | 5 | 8 | |
| Growth/Recovery | 8 | 5 | 9 | 6 | 9 | |
| Availability/Shelf Life | 6 | 6 | 3 | 9 | 8 | |
| Cost/ Inexpensiveness | 5 | 5 | 2 | 5 | 2 | |
| Sum of Weighted Products | 610 | 361 | 450 | 317 | 470 | |
| Total/Rank | 610 | 361 (#3) | 450 (#2) | 317 (#4) | 470 (#1) |
Based on the evaluation matrix, the best product to be used for the blood vessel replacement rank as TEVG being first, with 470/610 points, Autologous Vessels in second, with 450/610 points, only 20 points lower, measuring less than a 3% difference. In third is the Synthetic Polymer with 361/610 points, representing roughly 18% lower than TEVG, and the Xenografts come in last with 317/610 points, which is 25% lower than TEVG.
TEVG ranked very high in 6 of the 7 categories, with resistance to infection and growth and recovery on the top with autologous vessels. However, it ranked among the lowest, also along with autologous vessels, in the cost of the harvest and production of the material. Due to its
overall strong performance, the engineered tissue is able to take advantage of the technology today in addressing each of the design factors with precision solution solving each individual category. Specifically for cardiac application, the structural and mechanical design is able to target the high-pressure environment of the arterial system and the low permeability that deals with the risk of infection or mechanical failure makes this category perform on par with the autologous vessel, which has traditionally posed to have the highest potential success rate. Furthermore, in a particular category of availability and shelf life, TEVG performed substantially higher than Autologous Vessels, which brought a close comparison to having a distinct advantage.
The second best candidate is the Autologous Vessels, which has been the recommended path mainly due to its superior performance in mechanical/structural integrity, resistance to infection, and compliance or having a low rejection risk. In particular, the growth and recovery of using autologous vessels have improved overtime due to the efforts and developments in preventing damage of structural and functional integrity of vascular endothelium during harvest, storage, and implantation. However, the downfall comes in the availability/shelf life, which scored among the lowest as the effort in harvesting the product remains having the patient’s body as the only source, and the cost of the harvesting procedure remains high, as it involves another major surgical procedure.
Synthetic polymers and xenografts are third and last with a 20-25% gap between them and TEVG and Autologous Vessels. Synthetic polymers in particular, despite scoring highest in longevity and durability, and a high score in structural integrity, performed quite low in the other five categories. Specifically in the resistance to infection and the compliance/low rejection, synthetic polymers does not present itself to be a suitable candidate, which is a major disadvantage of polymers such as PTFE, and also structural failure found in the synthetic tissue PU, which is linked to enzymatic attacks, oxidative stress, and stress crackling, leading to infection. Xenografts scored among the lowest in many categories, even comparing to synthetic polymers. However, it performed marginally better in the resistance to infection and compliance/low rejection categories. This material shows a distinct major advantage in its availability/shelf life and the cost of the product. However, these two advantages do not outweigh the low scores in the other five categories, particularly with its lowest score in the longevity and durability performance.
Summary
This assignment served as the first step in developing a novel coronary artery bypass material for an elderly patient, Sally Smith. The first part served as a general research on available surgical procedures for Sally’s condition. The second part involves an in-depth research on current replacement vessel materials and their design and specific properties, particularly in comparison to native tissue found for cardiac applications. Benefits and limitations of the application of each material is weighted for their practicality and each is compared according to the seven criteria for a successful product. In future assignments, these criteria will serve as the design intent which will serve as a basis in designing a novel bypass material.
References
IMAGE REFERENCES:
Figure 5: ResearchGate. https://www.researchgate.net/figure/A-diagram-showing-a-saphenous-vein-graft-SVG-anastomo sed-end-to-side-to-the-left_fig3_312900853
Leave a comment